Health care benefits
Once we accept your claim, we will cover the cost of the health care services and supplies that are considered reasonably necessary to treat your injuries. This may include medical treatments, hospitalization, medical supplies, rehabilitation, and medications.
If you receive medical treatments related to your claim before we’ve accepted your claim, you may be asked to pay for them directly. If your claim is later accepted, you can contact your treatment provider to request reimbursement. They will normally bill us directly for all your treatments.
Once we accept your claim, your health care provider should bill us for any treatment related to your claim. You should not have to pay any fees.
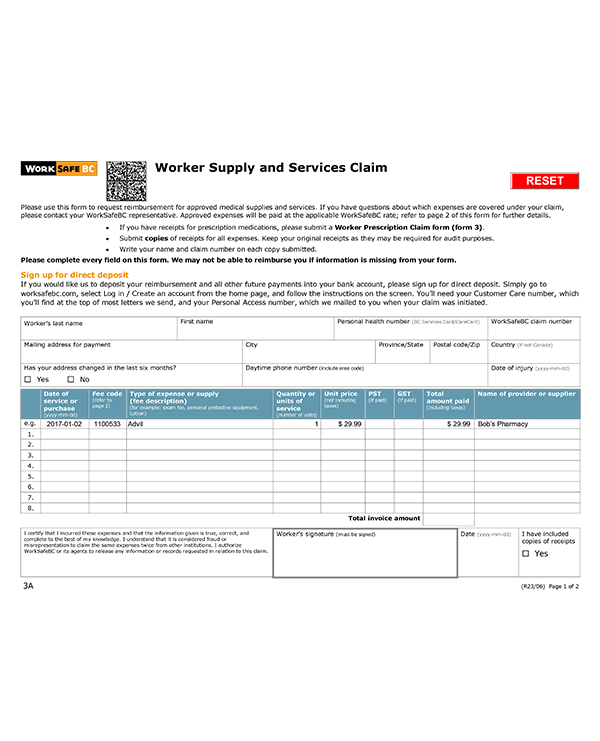
If you do pay for treatments, and you pay more than what we’ve negotiated with the health care provider, we may not be able to reimburse you for the extra costs. We are only able to pay the amount negotiated in the contract with the provider (the established rates are available on page 2 of Form 3A — Worker Supply and Service Claim Form). If you or your treatment provider have any questions about reimbursement, please contact our Payment Services team.
If you need physiotherapy, you should visit one of the service providers who have a contract with us in your region. Be sure to explain that your injury is work-related.
By choosing one of our contracted physiotherapists, you can get an initial assessment even before we accept your claim. The physiotherapist will also discuss how your injury affects your ability to do your job. They will bill us directly for this assessment.
If you choose a physiotherapist who has not contracted with us, you will have to pay for your visit. You can then seek reimbursement from us. Please keep in mind that we will reimburse you at established rates and you will be responsible for any difference (the established rates are available on page 2 of Form 3A — Worker Supply and Service Claim Form).
Please follow the guidelines below to receive treatment from a registered massage therapist (RMT). In all cases, be sure to tell the treatment provider that your injury is work-related.
- You will need a referral from your physician before seeking treatment.
- Once we accept your claim, you can receive up to six treatments within the first eight weeks from the date of your injury.
- If your treatment extends beyond eight weeks from the date of your injury, your massage therapist will need to contact us for approval.
- We recommend that you choose a provider who will bill directly to WorkSafeBC and submit reports. To find an RMT, please visit the Registered Massage Therapists Association of BC website and use the WorkSafeBC filter.
- If you choose a provider who does not bill us directly, you will have to pay for your visit and then seek reimbursement from us. Please keep in mind that we will reimburse you at pre-determined rates and you will be responsible for any difference (the established rates are available on page 2 of Form 3A — Worker Supply and Service Claim Form).
Specific guidelines exist for a variety of other health care treatments. In all cases, be sure to tell the treatment provider that your injury is work-related.
- Chiropractor, Acupuncture, or Naturopath: You do not need a referral for treatment. If you choose a provider who does not bill us directly, you will have to pay for your visit and then seek reimbursement from us. Please keep in mind that we will reimburse you at established rates and you will be responsible for any difference (the rates are available on page 2 of Form 3A — Worker Supply and Service Claim Form).
- Dental work: In all cases except emergencies, your case manager must approve treatment before you can receive it.
- Hospital services: Your benefits include emergency room visits, short- and long-term stays, day surgery, dressing changes, casting, and diagnostic imaging such as X-rays, CT scans, and MRIs.
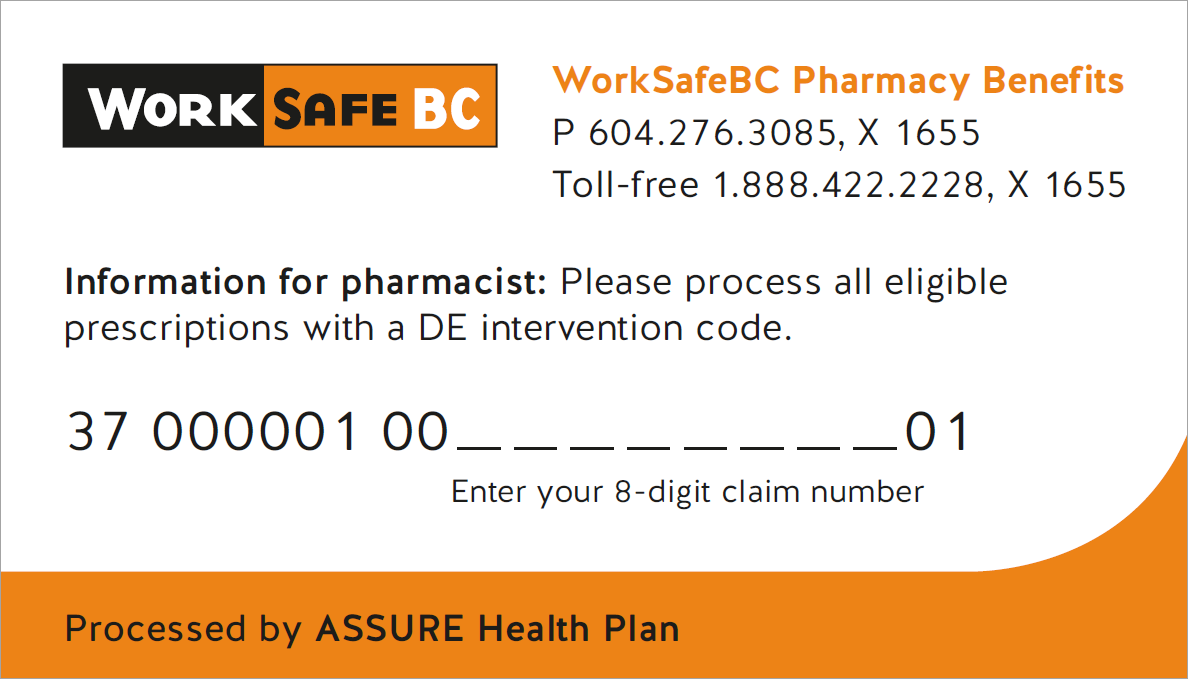
We will pay for prescriptions to treat conditions related to your accepted claim. You will receive a pharmacy card once your claim is accepted, which you can use to pay for your pre-approved prescriptions. If you haven’t received it yet, you can show the pharmacy this WorkSafeBC Pharmacy Benefits Card to pay for your pre-approved prescriptions. When you present the card to the pharmacist, you’ll also need to provide your claim number.
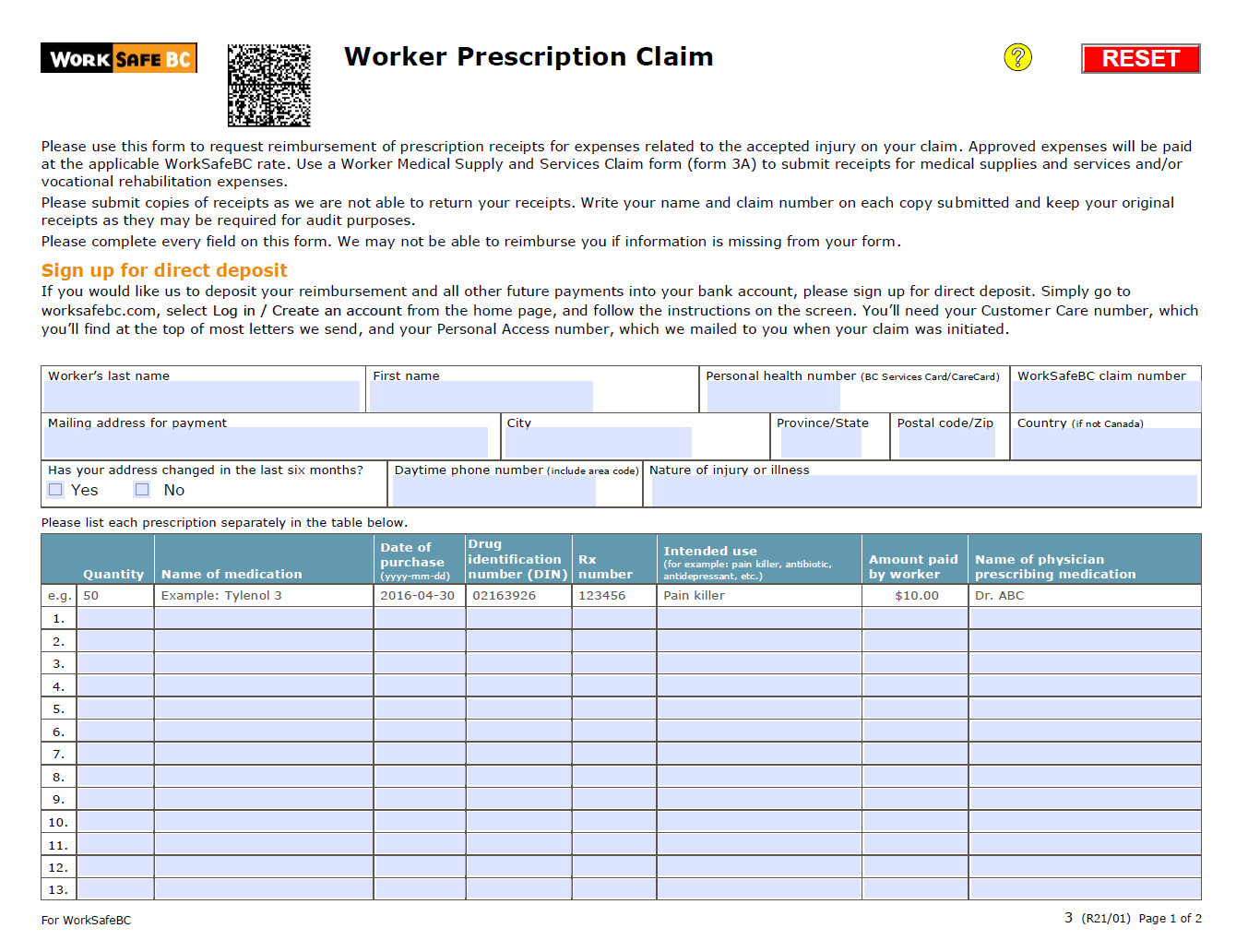
If you need to get reimbursed for your approved prescriptions, download and complete our Worker Prescription Claim (Form 3). Make sure you include your claim number.
Send us the form, along with a copy of your original pharmacy receipt (not the store cash register receipt). Please keep the original receipts as we may ask to see them at later date.
You can fax or mail the form to us. Our contact information is at the bottom of the form.
We will pay for approved health care goods and services on your accepted claim. To request reimbursement for your expenses, please download and complete our Worker Supply and Services Claim (Form 3A).
Be sure to complete all fields in the form and attach copies of your receipts with your name and claim number on each copy submitted. Please keep the original receipts as we may ask to see them.
You can fax or mail the form to us. Our contact information is at the bottom of the form.
We will pay for approved claim-related travel on your accepted claim. This can include reimbursement for mileage, airfare, hotels, ferry fares, taxis, or parking receipts.
You can request mileage reimbursement if you drive over 20 km one way for a claim-related appointment. Mileage is payable starting at 21 km (one way, or 41 km round trip). Trips must meet the minimum distance requirement to be paid. If you travel to see a provider when there is a qualified service provider closer to your home, mileage may not be paid.
To submit a request for reimbursement for a claim-related travel expense, please email Travel@worksafebc.com with the following information:
- Name
- Claim number
- Reason for travel
- Date(s) of travel
- Time of appointment
- Physical home address (PO boxes are not accepted)
- Copies of all applicable receipts. This can include receipts for airfare, hotels, ferry fares, taxis, and parking.
Questions?
If you have any questions, please call us at 604.276.5115 or 1.877.646.5115, Monday to Friday from 7:30 a.m. to 4:30 p.m.
Please note: The email address above is for reimbursement submissions only. If you need travel arranged for a future appointment, call us at the above number.